Healthcare data exchange is the backbone of modern medical innovation, enabling the seamless flow of health information across disparate systems and providers. By leveraging standardized protocols like HL7 FHIR for APIs and HL7 v2 for legacy messaging, organizations can break down data silos within EHRs like Epic and Cerner.
For AI professionals, mastering these standards is not just a technical requirement—it is a strategic necessity to secure the high-quality, HIPAA-compliant datasets required to train enterprise-grade models and drive clinical ROI.
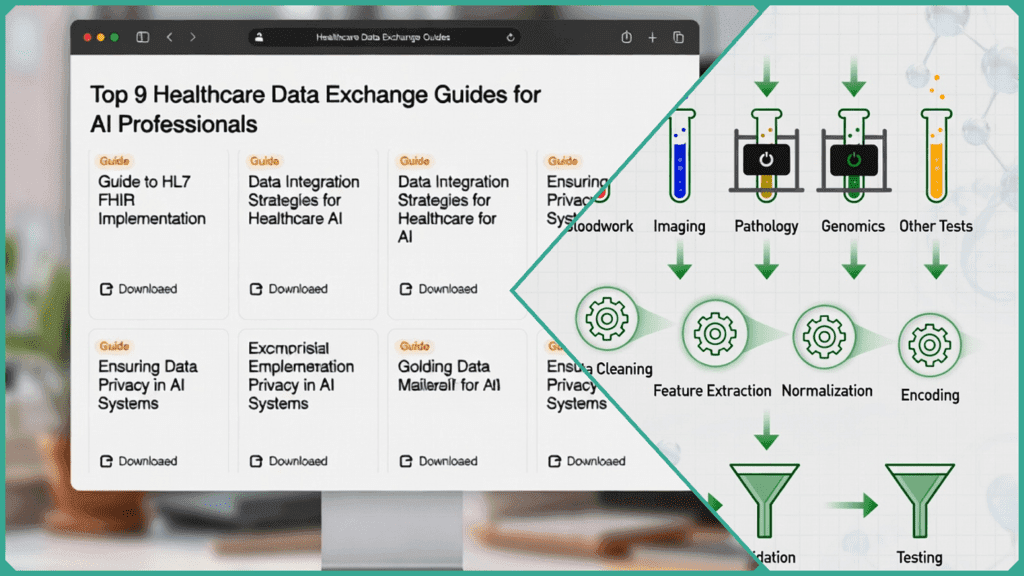
Top 9 Healthcare Data Exchange Guides
These guides provide the essential frameworks for AI professionals to ingest, normalize, and secure data from EHRs, imaging, and genomic pipelines.
FHIR (Fast Healthcare Interoperability Resources)
The industry gold standard. It uses a RESTful API approach, making it the preferred method for real-time AI ingestion. It breaks down patient records into “Resources” (e.g., Medication, Observation), allowing AI models to query only the specific data points they need.
HL7 v2
A legacy but ubiquitous message-based protocol. It is still the “workhorse” for real-time triggers in hospitals, such as lab results and patient admissions. AI professionals use this primarily for building “Early Warning” models that need to react to live hospital events.
OMOP Common Data Model (CDM)
While FHIR is for exchange, OMOP is the premier guide for AI research. It standardizes disparate data into a unified format, allowing a single AI model to be trained or validated across multiple international hospital databases without changing the code.
DICOM (Digital Imaging and Communications in Medicine)
The universal standard for medical imaging (MRI, CT, X-ray). Beyond just the image, the DICOM header contains vital metadata (tags) essential for training computer vision models, such as slice thickness and equipment settings.
USCDI (United States Core Data for Interoperability)
A roadmap of standardized data classes (like “Goals” or “Social Determinants of Health”) that all certified EHRs in the US must be able to share. This is the “dictionary” AI professionals use to know what data is guaranteed to be available in a structured format.
SMART on FHIR
A security and integration framework that allows AI apps to run directly inside an EHR (like Epic or Cerner). It provides a “plug-and-play” guide for developers to ensure their AI tool can launch with the correct patient context and security permissions.
SNOMED CT & LOINC
The “languages” of healthcare. SNOMED CT provides clinical terminology (e.g., specific disease types), while LOINC standardizes lab and observation codes. AI models require these for semantic interoperability—ensuring that “Blood Sugar” in one system is recognized as the same value in another.
FHIR Bulk Data Access (Flat FHIR)
Essential for Large Language Model (LLM) training. Instead of querying one patient at a time, this guide outlines how to export “bulk” datasets (thousands of patients at once) from an EHR into a data lake for massive-scale AI training.
HIPAA Security Rule (for Data in Transit)
The definitive guide for technical safeguards. For AI professionals, this means implementing end-to-end encryption, multi-factor authentication, and robust audit logs to ensure that data exchange doesn’t result in a PHI breach.
How Does FHIR Work in Data Exchange?
FHIR (Fast Healthcare Interoperability Resources) is more than just a data format; it is a standardized API framework that allows systems to communicate using modern web languages. For an AI professional, FHIR transforms a messy EHR into a structured, queryable database.
The Building Blocks: Resources
FHIR breaks down health data into modular units called Resources. Instead of sending a massive, monolithic file, systems exchange specific “packets” of information.
- Patient: Demographics (name, gender, DOB).
- Observation: The core of AI data—vitals (blood pressure, heart rate), lab results, and social determinants.
- Condition: Diagnoses and clinical problems.
- MedicationRequest: Orders and prescriptions.
The Exchange Mechanism: RESTful APIs
FHIR utilizes RESTful APIs, meaning it uses standard HTTP commands to move data. This is the same technology used by modern web apps like Spotify or Uber, making it highly accessible for software engineers.
GET /Patient/123: Retrieves the record for a specific patient.GET /Observation?patient=123&code=29463-7: Pulls specific weight measurements (using a LOINC code) for an AI weight-trend model.
Data Representation: JSON and XML
Resources are serialized into JSON (the favorite for AI/ML pipelines) or XML. Because JSON is natively supported by Python and most data science libraries, AI professionals can ingest FHIR data directly into dataframes with minimal pre-processing.
Example FHIR JSON (Observation):
{ “resourceType”: “Observation”, “status”: “final”, “code”: { “coding”: [{ “system”: “http://loinc.org”, “code”: “85354-9” }] }, “subject”: { “reference”: “Patient/example” }, “valueQuantity”: { “value”: 120, “unit”: “mmHg” } }Real-Time Feeds vs. Bulk Data
- Real-Time (SMART on FHIR): Ideal for “at-the-elbow” AI tools, such as a bedside sepsis predictor that pulls v_itals_ the moment they are recorded in the EHR.
- Bulk Data (FHIR Bulk Data API): Crucial for Strategy and Training. This allows AI teams to export hundreds of thousands of patient records at once (often called “Flat FHIR”) to train Large Language Models (LLMs) or population health algorithms.
What Is the Role of USCDI?
While FHIR provides the “pipes” for data exchange, the United States Core Data for Interoperability (USCDI) defines the “water” flowing through them. It is the mandatory minimum set of data classes that all certified Health IT must be able to exchange.
The “Baseline” for AI Training
For AI professionals, USCDI is a guarantee. If a system is ONC-certified, you can trust that these data classes—such as immunizations (which currently see 92% availability across health information exchanges)—will be available in a structured, predictable format. This drastically reduces the time spent on manual data cleaning and mapping.
Mandatory Transition in 2026: USCDI v3
As of January 1, 2026, the HTI-1 Final Rule mandates that USCDI v3 replace v1 as the baseline standard for all certified Health IT. This version nearly doubles the required data elements, providing AI models with a much richer context of the patient’s life.
Advancing Health Equity with SDOH
A critical strategic shift in USCDI v3 is the requirement for Social Determinants of Health (SDOH) data. Mandatory classes now include:
- SDOH Assessments: Standardized screening results for food insecurity or housing instability.
- SDOH Problems/Goals: Identified social risks and the interventions planned to address them.
- Health Status: Inclusion of disability status, mental/cognitive function, and pregnancy status.
Reducing Silos in Population Health
By pairing USCDI with FHIR, AI professionals can conduct population health studies with higher accuracy. Instead of being limited to clinical vitals, models can now integrate socioeconomic factors to identify bias and improve the equity of predictive algorithms. This is essential for meeting new “Algorithm Transparency” requirements that demand AI be validated for fairness across diverse demographics.
Why Is Data Normalization Critical for AI?
In healthcare, data normalization is the process of mapping disparate information from various sources into a unified, “common language.” Without it, AI models fall prey to the GIGO (Garbage In, Garbage Out) principle, in which inconsistent data leads to biased or inaccurate predictions.
The “Language Gap” in Healthcare
EHR systems often use local, non-standard codes for clinical concepts. For example, three different hospitals might record “Serum Potassium” using three different internal IDs.
- The Solution: Mapping these to LOINC (for labs) and SNOMED CT (for clinical findings).
- The Impact: Recent studies show that mapping local lab codes to LOINC can reduce dimensionality by 73%, consolidating thousands of idiosyncratic codes into a few hundred standardized concepts that an AI can actually understand.
Boosting Model Accuracy
Normalized data ensures that an AI model trained on Data from “Hospital A” can perform reliably at “Hospital B.”
- Automated Pipelines: AI-assisted normalization tools are now being used to automate these pipelines, achieving up to 90%+ accuracy in auto-coding medical terms.
- Precision: High-quality, normalized datasets have been shown to improve diagnostic accuracy by up to 30% in predictive analytics, specifically for high-stakes cases like sepsis detection or mortality prediction.
Efficiency Gains for ML Engineers
According to internal audits at Skilldential, the “prep” phase is where most AI projects stall. ML engineers often spend 80% of their time cleaning “messy” EHR data rather than building models.
- The “FHIR” Advantage: Implementing FHIR-native pipelines eliminates the need for institution-specific preprocessing.
- Result: Organizations using automated FHIR pipelines report 40% to 80% faster data preparation, allowing teams to move from raw extraction to model training in hours rather than weeks.
Reducing Bias and Improving Equity
Standardization allows for the inclusion of Social Determinants of Health (SDOH). When data is normalized across demographics, AI models can more easily identify and mitigate algorithmic bias, ensuring that “missing” data isn’t misinterpreted as “normal” data.
Standards Comparison Matrix
Understanding which standard to use depends on your specific use case, whether you are training a computer vision model or building a real-time clinical dashboard.
| Standard | Primary Use Case | AI Fit | Compliance & Security Focus |
| FHIR | Real-time clinical APIs & Apps | High: JSON structure is perfect for Python/ML ingestion. | HIPAA/GDPR: Supports OAuth2 and granular access. |
| HL7 v2 | Legacy messaging (Labs, ADT) | Medium: Requires parsing; best for real-time triggers. | Basic: Usually relies on secure VPN/Tunneling. |
| DICOM | Radiology & Medical Imaging | High: Essential for Computer Vision & Diagnostics. | De-identification: Critical for removing PHI from headers. |
| USCDI | Mandatory Core Data Sets | High: Standardized “features” for RWE & Analytics. | ONC Certification: Guaranteed data availability by law. |
| DirectTrust | Secure EHR-to-EHR “Email” | Low-Medium: Best for “pushing” PDFs or CCDAs. | PKI Encryption: Uses digital certificates for trust. |
| OMOP CDM | Large-scale Research & LLMs | High: Unifies data across different hospital networks. | Standardization: Focuses on research reproducibility. |
Strategic Highlights for 2026:
- The Rise of “Flat FHIR”: For AI Business & Strategy, the Bulk Data Access (Flat FHIR) is now the standard for training Large Language Models (LLMs) on institutional data without overloading live EHR servers.
- Privacy-Preserving AI: DICOM and FHIR are increasingly paired with Federated Learning frameworks. This allows AI professionals to train models on decentralized data without the sensitive PHI ever leaving the hospital’s firewall.
- Imaging Metadata: For AI Career Paths in diagnostics, mastering the DICOM “header” is as important as the pixels themselves, as it contains the equipment parameters that can cause “batch effects” or bias in your models.
What Challenges Do Compliance Officers Face?
In 2026, the role of a Compliance Officer has shifted from a “gatekeeper” to a “governance architect.” As AI adoption accelerates, these professionals must balance the hunger for high-utility data with increasingly strict global regulations.
The primary friction point for compliance in 2026 is the Privacy-Utility Tradeoff: How do you strip enough data to protect a patient’s identity without making the dataset useless for an AI model?
The De-identification Paradox
Traditional de-identification (removing names, SSNs, etc.) is no longer enough. Modern AI, through pattern analysis, can often re-identify individuals using “anonymous” longitudinal data (e.g., matching a unique sequence of prescriptions and visit dates).
- The Strategy: Officers are moving toward Differential Privacy—adding mathematical “noise” to datasets so that individual records cannot be singled out, while the overall statistical trends remain accurate for AI training.
Global Sovereignty and Consent Tracking
With regulations like the EU AI Act and GDPR now standardizing cross-border flows, tracking patient consent has become a massive logistical hurdle.
- The Solution: Blockchain-backed Audit Trails. By recording every data access and modification on a decentralized ledger, officers create an immutable record. If a patient revokes consent, the blockchain ensures that their data is instantly flagged and removed from active training pipelines, providing a “tamper-proof” audit for regulators.
Compliance-as-Code (CaC)
In 2026, manual audits are being replaced by Automated Compliance Pipelines.
- How it works: Compliance requirements are “baked” directly into the MLOps lifecycle.
- Automated Gatekeeping: If a data scientist attempts to ingest a dataset that lacks proper USCDI v3 formatting or proof of consent, the pipeline automatically halts the ingestion.
- Result: This reduces human error—like a human coder making a one-time mistake versus an AI model incorrectly processing thousands of records—and cuts audit preparation time by up to 50%.
Algorithmic Bias and Ethical Oversight
Compliance officers now oversee Fairness Audits. They must ensure that the “Exchange Guides” being used include diverse datasets (including SDOH). Failure to do so doesn’t just result in a poor model; it now carries legal liability under the new 2026 health equity mandates.
How Does Exchange Improve Outcomes?
Ultimately, the strategic exchange of data isn’t just about technical compliance—it’s about moving the needle on patient health and organizational efficiency. When data flows seamlessly, AI can move from a “research project” to a real-time clinical partner.
For AI professionals, the goal of data interoperability is to provide the right insights at the moment they can make the most difference.
Clinical Impact: “At-the-Elbow” Sepsis Detection
Sepsis remains a leading cause of hospital mortality. Traditional detection relies on manual checks of vital signs, often resulting in delayed treatment.
- The Exchange Advantage: By using FHIR to pull real-time feeds of vitals, labs, and nursing notes, AI models can detect the subtle signs of sepsis up to 12 hours earlier than human observation alone.
- The Outcome: Every hour of delayed treatment increases the risk of death by nearly 8%. Real-time data exchange allows AI to trigger alerts directly in the clinician’s workflow, literally saving lives at the bedside.
2. Operational Impact: Automating Prior Authorization
Prior authorization (PA) is often cited as the #1 administrative burden for physicians, frequently leading to treatment delays of days or weeks.
- The AI Solution: In 2026, the CMS-0057-F mandate requires payers to use FHIR APIs for prior authorizations. AI tools can now automatically “crawl” a patient’s EHR, pull the specific USCDI v3 data needed for a request, and submit it instantly.
- The Outcome: This reduces the PA cycle from weeks to seconds, cutting administrative costs by an estimated $15 billion over the next decade and ensuring patients start life-saving therapies without delay.
Ethical Impact: Boosting Equity with SDOH Data
AI is only as fair as the data it is fed. Historically, marginalized populations have been underrepresented in clinical datasets.
- The Strategy: By integrating Social Determinants of Health (SDOH)—such as housing stability and food security—into the standard data exchange, AI professionals can build models that identify “hidden” risks.
- The Outcome: AI can help healthcare systems proactively deploy resources (like community health workers or transportation vouchers) to at-risk populations. This moves healthcare from a “one-size-fits-all” model to an equitable, proactive system that addresses the root causes of health disparities.
To succeed in the 2026 healthcare AI landscape, you must view these 9 guides not as hurdles, but as accelerators. Mastering the flow of data—from legacy HL7 messages to modern FHIR resources—is what allows you to build models that are not only technically impressive but clinically indispensable.
Healthcare Data Exchange FAQs
What is Healthcare Data Exchange?
Healthcare data exchange is the electronic transfer of health information between disparate systems, providers, and organizations using standardized protocols like FHIR and HL7. It breaks down data silos to enable real-time interoperability, supporting AI/ML training with normalized EHR, imaging, and genomics data from sources like Epic systems. This process ensures high-quality inputs critical for robust models while adhering to privacy rules.
Is FHIR Mandatory for US Health IT?
No, FHIR is not universally mandatory, but ONC certification for health IT systems requires support for USCDI data elements via FHIR APIs starting in 2026. This facilitates seamless exchange across certified EHRs, allowing AI tools to access structured patient data without custom mappings. It promotes a learning health system but allows legacy HL7 v2 as a bridge.
How Does HIPAA Apply to Data Exchange?
HIPAA’s Security Rule requires encryption (e.g., TLS 1.3), access controls, and audit logs for PHI during transit and rest in data exchanges. For AI pipelines, this means de-identifying data per Safe Harbor methods before training to avoid breaches, with violations risking fines up to $50,000 per incident. Compliance-by-design tools automate consent tracking in FHIR-based flows.
What is USCDI v3?
USCDI v3 is the ONC’s standardized dataset expanding on prior versions to include social determinants of health (SDOH), behavioral health, and clinical notes for interoperable exchange. It defines 72 data classes transportable via FHIR, enabling secondary uses like population health AI and real-world evidence generation. Adopted in 2026, it mandates diverse data for equity in ML models.
Can AI Automate Data Mapping?
Yes, AI-driven tools like transformer models automate mapping disparate formats (e.g., EHR variances) to standards such as LOINC/SNOMED, reducing manual effort by 30-50% and boosting data quality. FHIR’s resource structure simplifies ingestion, while ML handles normalization for “garbage in, garbage out” prevention in training datasets. In Skilldential audits, DevOps teams saw 40% faster pipelines post-implementation.
In Conclusion
In 2026, the success of a healthcare AI professional is measured not just by the complexity of their models but by the integrity of their data pipelines. These top 9 guides represent more than technical specifications; they are the strategic blueprints for building trustworthy, scalable, and equitable health technology.
By mastering standards like FHIR and USCDI v3, you transition from “cleaning data” to “architecting innovation.” As interoperability becomes the center of the healthcare ecosystem, the ability to move information seamlessly between systems will be the primary driver of clinical ROI and improved patient outcomes.
Final Checklist for AI Professionals:
- Audit Your Ingestion: Are you using FHIR for real-time clinical data and OMOP for your research-at-scale?
- Verify Normalization: Have you automated the mapping of local codes to LOINC and SNOMED CT to prevent “Garbage In, Garbage Out”?
- Future-Proof with USCDI v3: Are your 2026 pipelines ready to ingest mandatory Social Determinants of Health (SDOH) data to ensure model equity?
- Prioritize Governance: Is compliance embedded directly into your MLOps pipeline to automate audit trails and consent tracking?
The barrier to entry for healthcare AI is no longer the algorithm—it is the data. Those who master the exchange will lead the next generation of medical discovery.
- Don’t Start a YouTube Channel with AI Until You Read This - January 29, 2026
- 9 Best Cisco Networking Academy Courses for Beginners - January 29, 2026
- 9 Common AI Training Data Biases You Should Know - January 29, 2026
Discover more from SkillDential | Your Path to High-Level AI Career Skills
Subscribe to get the latest posts sent to your email.
